What Layer Can Change Blood Vessel Diameter by Vasodilation and Vasoconstriction?
Learning Objectives
By the end of this section, you volition be able to:
- Compare and contrast the 3 tunics that brand up the walls of most blood vessels
- Distinguish betwixt elastic arteries, muscular arteries, and arterioles on the basis of structure, location, and function
- Describe the basic structure of a capillary bed, from the supplying metarteriole to the venule into which it drains
- Explain the structure and function of venous valves in the large veins of the extremities
Blood is carried through the body via blood vessels. An avenue is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels. Somewhen, the smallest arteries, vessels called arterioles, further branch into tiny capillaries, where nutrients and wastes are exchanged, and and so combine with other vessels that get out capillaries to form venules, pocket-size blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the centre.
Arteries and veins transport blood in two singled-out circuits: the systemic circuit and the pulmonary circuit. Systemic arteries provide blood rich in oxygen to the body's tissues. The blood returned to the center through systemic veins has less oxygen, since much of the oxygen carried by the arteries has been delivered to the cells. In contrast, in the pulmonary excursion, arteries carry blood low in oxygen exclusively to the lungs for gas exchange. Pulmonary veins then render freshly oxygenated blood from the lungs to the heart to exist pumped back out into systemic apportionment. Although arteries and veins differ structurally and functionally, they share certain features.
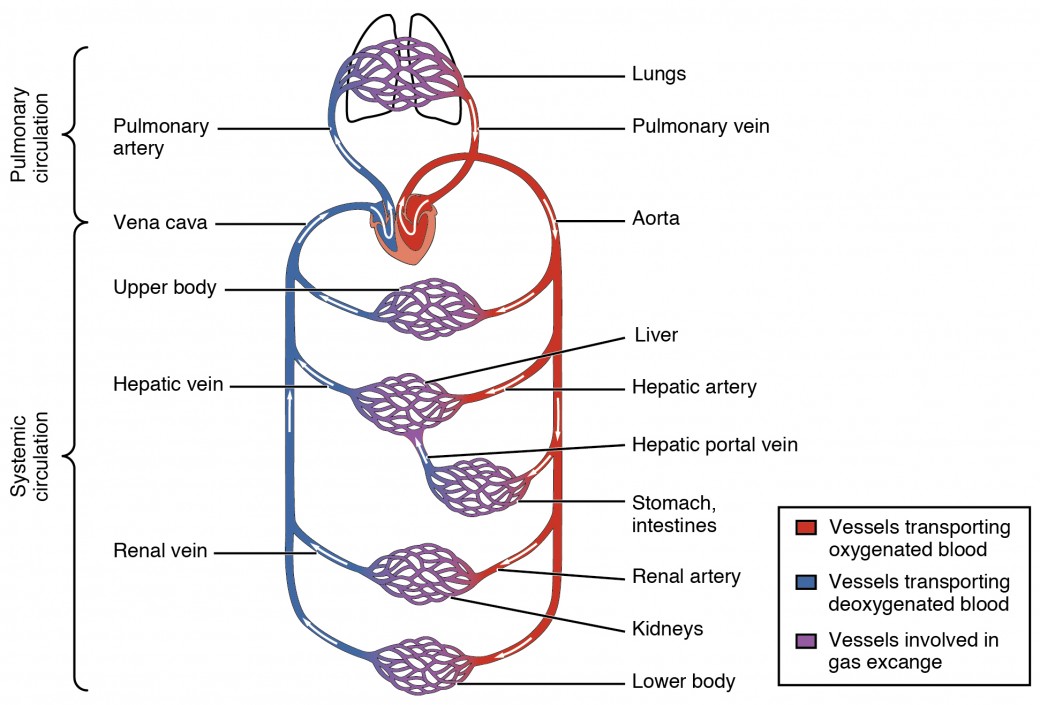
Figure 1. The pulmonary circuit moves blood from the right side of the heart to the lungs and back to the heart. The systemic circuit moves claret from the left side of the heart to the head and torso and returns it to the correct side of the heart to repeat the bicycle. The arrows indicate the direction of claret flow, and the colors show the relative levels of oxygen concentration.
Shared Structures
Different types of blood vessels vary slightly in their structures, just they share the same general features. Arteries and arterioles have thicker walls than veins and venules because they are closer to the middle and receive blood that is surging at a far greater force per unit area (Effigy ii). Each type of vessel has a lumen—a hollow passageway through which blood flows. Arteries have smaller lumens than veins, a feature that helps to maintain the pressure of blood moving through the system. Together, their thicker walls and smaller diameters give arterial lumens a more rounded appearance in cross department than the lumens of veins.
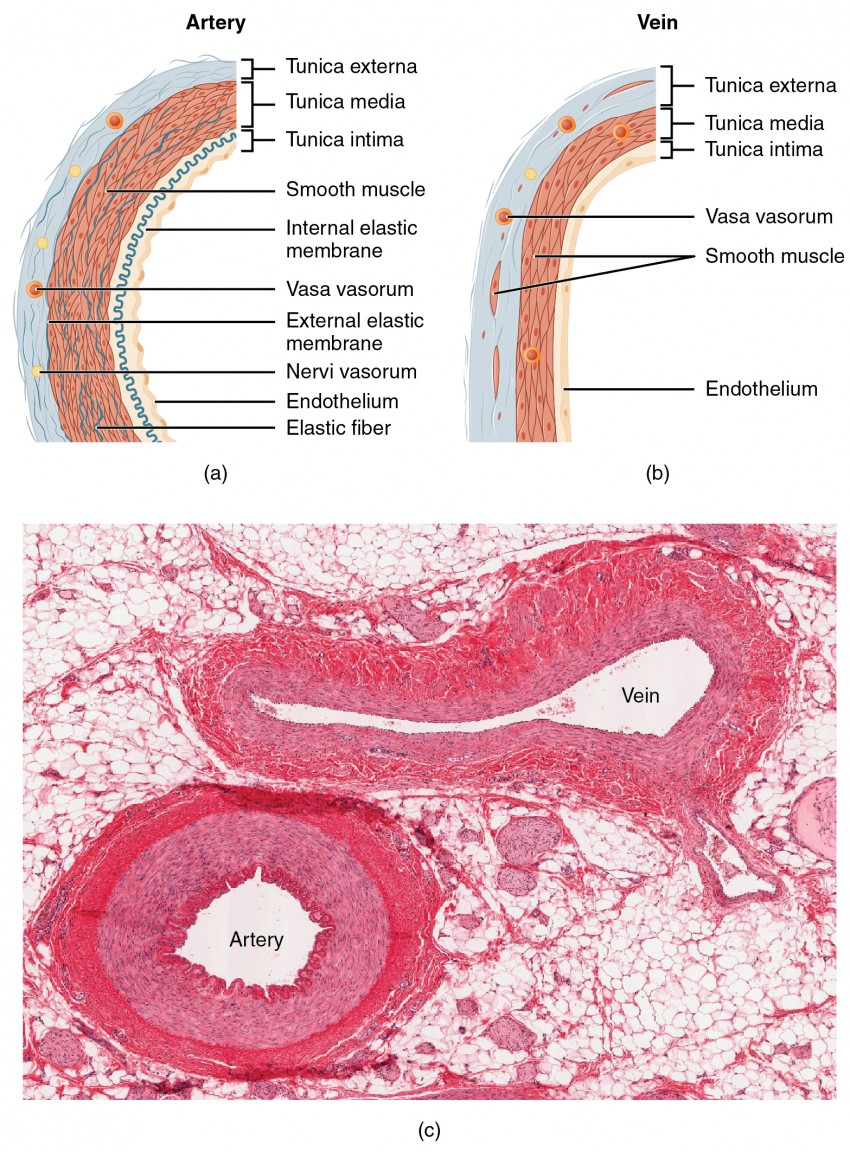
Figure 2. (a) Arteries and (b) veins share the same general features, but the walls of arteries are much thicker because of the higher pressure level of the blood that flows through them. (c) A micrograph shows the relative differences in thickness. LM × 160. (Micrograph provided by the Regents of the Academy of Michigan Medical School © 2012)
By the time blood has passed through capillaries and entered venules, the pressure initially exerted upon it by heart contractions has diminished. In other words, in comparison to arteries, venules and veins withstand a much lower pressure level from the blood that flows through them. Their walls are considerably thinner and their lumens are correspondingly larger in diameter, allowing more than blood to catamenia with less vessel resistance. In addition, many veins of the body, particularly those of the limbs, comprise valves that assist the unidirectional flow of claret toward the center. This is critical because blood flow becomes sluggish in the extremities, as a result of the lower force per unit area and the effects of gravity.
The walls of arteries and veins are largely composed of living cells and their products (including collagenous and rubberband fibers); the cells require nourishment and produce waste matter. Since blood passes through the larger vessels relatively speedily, there is limited opportunity for claret in the lumen of the vessel to provide nourishment to or remove waste from the vessel's cells. Farther, the walls of the larger vessels are too thick for nutrients to diffuse through to all of the cells. Larger arteries and veins contain small blood vessels within their walls known equally the vasa vasorum—literally "vessels of the vessel"—to provide them with this critical exchange. Since the pressure within arteries is relatively high, the vasa vasorum must function in the outer layers of the vessel or the pressure exerted by the claret passing through the vessel would collapse information technology, preventing whatsoever commutation from occurring. The lower pressure within veins allows the vasa vasorum to be located closer to the lumen. The restriction of the vasa vasorum to the outer layers of arteries is idea to exist one reason that arterial diseases are more than common than venous diseases, since its location makes it more than difficult to nourish the cells of the arteries and remove waste products. At that place are likewise infinitesimal nerves within the walls of both types of vessels that control the contraction and dilation of smooth muscle. These minute nerves are known equally the nervi vasorum.
Both arteries and veins accept the same iii distinct tissue layers, called tunics (from the Latin term tunica), for the garments kickoff worn by aboriginal Romans; the term tunic is likewise used for some modernistic garments. From the most interior layer to the outer, these tunics are the tunica intima, the tunica media, and the tunica externa. Table 1 compares and contrasts the tunics of the arteries and veins.
| Tabular array 1. Comparing of Tunics in Arteries and Veins | ||
|---|---|---|
| Arteries | Veins | |
| Full general appearance | Thick walls with minor lumens; Generally appear rounded | Thin walls with large lumens; Generally appear flattened |
| Tunica intima | Endothelium commonly appears wavy due to constriction of smooth muscle; Internal elastic membrane present in larger vessels | Endothelium appears polish; Internal rubberband membrane absent |
| Tunica media | Unremarkably the thickest layer in arteries; Smooth musculus cells and elastic fibers predominate (the proportions of these vary with distance from the middle); External rubberband membrane nowadays in larger vessels | Unremarkably thinner than the tunica externa; Smooth musculus cells and collagenous fibers predominate; Nervi vasorum and vasa vasorum nowadays; External elastic membrane absent-minded |
| Tunica externa | Normally thinner than the tunica media in all only the largest arteries; Collagenous and rubberband fibers; Nervi vasorum and vasa vasorum present | Commonly the thickest layer in veins; Collagenous and smooth fibers predominate; Some smooth musculus fibers; Nervi vasorum and vasa vasorum present |
Tunica Intima
The tunica intima (too chosen the tunica interna) is equanimous of epithelial and connective tissue layers. Lining the tunica intima is the specialized simple squamous epithelium called the endothelium, which is continuous throughout the entire vascular system, including the lining of the chambers of the heart. Harm to this endothelial lining and exposure of blood to the collagenous fibers below is one of the primary causes of clot formation. Until recently, the endothelium was viewed just equally the boundary betwixt the blood in the lumen and the walls of the vessels. Recent studies, however, have shown that it is physiologically critical to such activities equally helping to regulate capillary substitution and altering blood period. The endothelium releases local chemicals chosen endothelins that tin constrict the shine muscle inside the walls of the vessel to increase blood pressure. Uncompensated overproduction of endothelins may contribute to hypertension (high claret pressure) and cardiovascular illness.
Side by side to the endothelium is the basement membrane, or basal lamina, that effectively binds the endothelium to the connective tissue. The basement membrane provides strength while maintaining flexibility, and it is permeable, allowing materials to pass through it. The thin outer layer of the tunica intima contains a small amount of areolar connective tissue that consists primarily of elastic fibers to provide the vessel with additional flexibility; it also contains some collagenous fibers to provide boosted forcefulness.
In larger arteries, there is also a thick, distinct layer of rubberband fibers known equally the internal elastic membrane (as well called the internal rubberband lamina) at the boundary with the tunica media. Similar the other components of the tunica intima, the internal elastic membrane provides structure while allowing the vessel to stretch. It is permeated with modest openings that let commutation of materials between the tunics. The internal elastic membrane is non apparent in veins. In improver, many veins, particularly in the lower limbs, incorporate valves formed by sections of thickened endothelium that are reinforced with connective tissue, extending into the lumen.
Nether the microscope, the lumen and the unabridged tunica intima of a vein will appear smooth, whereas those of an artery volition unremarkably appear wavy considering of the fractional constriction of the smoothen musculus in the tunica media, the adjacent layer of claret vessel walls.
Tunica Media
The tunica media is the substantial heart layer of the vessel wall (see Figure 2). Information technology is more often than not the thickest layer in arteries, and it is much thicker in arteries than it is in veins. The tunica media consists of layers of smooth muscle supported by connective tissue that is primarily made up of elastic fibers, near of which are arranged in circular sheets. Toward the outer portion of the tunic, there are as well layers of longitudinal musculus. Contraction and relaxation of the circular muscles decrease and increase the diameter of the vessel lumen, respectively. Specifically in arteries, vasoconstriction decreases blood flow as the smooth muscle in the walls of the tunica media contracts, making the lumen narrower and increasing blood force per unit area. Similarly, vasodilation increases blood flow as the smooth musculus relaxes, allowing the lumen to widen and blood pressure to drop. Both vasoconstriction and vasodilation are regulated in part by small vascular nerves, known equally nervi vasorum, or "fretfulness of the vessel," that run within the walls of claret vessels. These are generally all sympathetic fibers, although some trigger vasodilation and others induce vasoconstriction, depending upon the nature of the neurotransmitter and receptors located on the target cell. Parasympathetic stimulation does trigger vasodilation besides as erection during sexual arousal in the external genitalia of both sexes. Nervous control over vessels tends to be more generalized than the specific targeting of individual blood vessels. Local controls, discussed later, account for this miracle. (Seek additional content for more information on these dynamic aspects of the autonomic nervous organisation.) Hormones and local chemicals as well control claret vessels. Together, these neural and chemical mechanisms reduce or increase claret catamenia in response to changing body conditions, from exercise to hydration. Regulation of both blood menses and claret pressure is discussed in detail afterward in this affiliate.
The polish muscle layers of the tunica media are supported by a framework of collagenous fibers that as well binds the tunica media to the inner and outer tunics. Forth with the collagenous fibers are large numbers of elastic fibers that appear as wavy lines in prepared slides. Separating the tunica media from the outer tunica externa in larger arteries is the external elastic membrane (also called the external rubberband lamina), which also appears wavy in slides. This structure is non usually seen in smaller arteries, nor is it seen in veins.
Tunica Externa
The outer tunic, the tunica externa (too called the tunica adventitia), is a substantial sheath of connective tissue composed primarily of collagenous fibers. Some bands of elastic fibers are found hither as well. The tunica externa in veins also contains groups of smooth muscle fibers. This is commonly the thickest tunic in veins and may be thicker than the tunica media in some larger arteries. The outer layers of the tunica externa are non distinct only rather blend with the surrounding connective tissue exterior the vessel, helping to agree the vessel in relative position. If yous are able to palpate some of the superficial veins on your upper limbs and try to move them, you will find that the tunica externa prevents this. If the tunica externa did not hold the vessel in place, any movement would probable result in disruption of claret flow.
Arteries
An avenue is a claret vessel that conducts claret away from the heart. All arteries have relatively thick walls that can withstand the high pressure of claret ejected from the middle. Nevertheless, those shut to the center have the thickest walls, containing a high percentage of elastic fibers in all iii of their tunics. This blazon of avenue is known as an elastic avenue (run across Figure 3). Vessels larger than 10 mm in diameter are typically elastic. Their abundant rubberband fibers allow them to expand, every bit blood pumped from the ventricles passes through them, and so to recoil after the surge has passed. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase and claret pressure would ascension to fifty-fifty higher levels, which would in turn require the center to pump harder to increase the volume of claret expelled past each pump (the stroke volume) and maintain adequate pressure and period. Avenue walls would have to become even thicker in response to this increased pressure. The rubberband recoil of the vascular wall helps to maintain the pressure slope that drives the blood through the arterial arrangement. An elastic artery is likewise known as a conducting artery, considering the large diameter of the lumen enables it to accept a large volume of blood from the heart and conduct it to smaller branches.

Figure iii. Comparing of the walls of an elastic artery, a muscular artery, and an arteriole is shown. In terms of scale, the bore of an arteriole is measured in micrometers compared to millimeters for elastic and muscular arteries.
Farther from the heart, where the surge of blood has dampened, the percent of rubberband fibers in an avenue's tunica intima decreases and the amount of smooth muscle in its tunica media increases. The artery at this point is described every bit a muscular artery. The bore of muscular arteries typically ranges from 0.1 mm to ten mm. Their thick tunica media allows muscular arteries to play a leading role in vasoconstriction. In dissimilarity, their decreased quantity of elastic fibers limits their ability to expand. Fortunately, considering the blood pressure has eased by the fourth dimension it reaches these more afar vessels, elasticity has become less important.
Observe that although the distinctions between elastic and muscular arteries are important, there is no "line of demarcation" where an rubberband artery suddenly becomes muscular. Rather, in that location is a gradual transition as the vascular tree repeatedly branches. In turn, muscular arteries branch to distribute blood to the vast network of arterioles. For this reason, a muscular artery is as well known every bit a distributing artery.
Arterioles
An arteriole is a very small artery that leads to a capillary. Arterioles take the same three tunics as the larger vessels, but the thickness of each is greatly diminished. The critical endothelial lining of the tunica intima is intact. The tunica media is restricted to i or two smooth muscle cell layers in thickness. The tunica externa remains just is very thin (run across Figure 3).
With a lumen averaging 30 micrometers or less in bore, arterioles are critical in slowing downward—or resisting—blood flow and, thus, causing a substantial driblet in blood pressure level. Because of this, you may see them referred to as resistance vessels. The musculus fibers in arterioles are normally slightly contracted, causing arterioles to maintain a consistent muscle tone—in this instance referred to every bit vascular tone—in a similar mode to the muscular tone of skeletal musculus. In reality, all blood vessels showroom vascular tone due to the partial contraction of smooth musculus. The importance of the arterioles is that they volition be the chief site of both resistance and regulation of blood pressure. The precise bore of the lumen of an arteriole at any given moment is determined by neural and chemical controls, and vasoconstriction and vasodilation in the arterioles are the primary mechanisms for distribution of blood flow.
Capillaries
A capillary is a microscopic channel that supplies blood to the tissues themselves, a process chosen perfusion. Substitution of gases and other substances occurs in the capillaries betwixt the claret and the surrounding cells and their tissue fluid (interstitial fluid). The diameter of a capillary lumen ranges from 5–10 micrometers; the smallest are just barely wide plenty for an erythrocyte to squeeze through. Flow through capillaries is ofttimes described as microcirculation.
The wall of a capillary consists of the endothelial layer surrounded by a basement membrane with occasional smooth muscle fibers. In that location is some variation in wall construction: In a large capillary, several endothelial cells bordering each other may line the lumen; in a small capillary, there may be only a unmarried cell layer that wraps around to contact itself.
For capillaries to office, their walls must be leaky, allowing substances to laissez passer through. There are iii major types of capillaries, which differ according to their degree of "leakiness:" continuous, fenestrated, and sinusoid capillaries.
Continuous Capillaries
The most common type of capillary, the continuous capillary, is found in near all vascularized tissues. Continuous capillaries are characterized by a complete endothelial lining with tight junctions betwixt endothelial cells. Although a tight junction is ordinarily impermeable and only allows for the passage of h2o and ions, they are oftentimes incomplete in capillaries, leaving intercellular clefts that allow for commutation of water and other very pocket-size molecules between the blood plasma and the interstitial fluid. Substances that can pass between cells include metabolic products, such as glucose, water, and small hydrophobic molecules like gases and hormones, as well equally various leukocytes. Continuous capillaries not associated with the encephalon are rich in ship vesicles, contributing to either endocytosis or exocytosis. Those in the brain are part of the claret-brain bulwark. Here, there are tight junctions and no intercellular clefts, plus a thick basement membrane and astrocyte extensions called end feet; these structures combine to prevent the move of nearly all substances.

Figure 4. The three major types of capillaries: continuous, fenestrated, and sinusoid.
Fenestrated Capillaries
A fenestrated capillary is 1 that has pores (or fenestrations) in addition to tight junctions in the endothelial lining. These make the capillary permeable to larger molecules. The number of fenestrations and their degree of permeability vary, however, according to their location. Fenestrated capillaries are common in the minor intestine, which is the primary site of food absorption, besides as in the kidneys, which filter the blood. They are as well found in the choroid plexus of the brain and many endocrine structures, including the hypothalamus, pituitary, pineal, and thyroid glands.
Sinusoid Capillaries
A sinusoid capillary (or sinusoid) is the least common type of capillary. Sinusoid capillaries are flattened, and they have extensive intercellular gaps and incomplete basement membranes, in addition to intercellular clefts and fenestrations. This gives them an appearance not unlike Swiss cheese. These very large openings allow for the passage of the largest molecules, including plasma proteins and fifty-fifty cells. Blood flow through sinusoids is very slow, allowing more fourth dimension for exchange of gases, nutrients, and wastes. Sinusoids are found in the liver and spleen, bone marrow, lymph nodes (where they carry lymph, not claret), and many endocrine glands including the pituitary and adrenal glands. Without these specialized capillaries, these organs would not be able to provide their myriad of functions. For instance, when bone marrow forms new blood cells, the cells must enter the blood supply and tin can just practise then through the large openings of a sinusoid capillary; they cannot pass through the pocket-sized openings of continuous or fenestrated capillaries. The liver likewise requires extensive specialized sinusoid capillaries in order to process the materials brought to it by the hepatic portal vein from both the digestive tract and spleen, and to release plasma proteins into circulation.
Metarterioles and Capillary Beds
A metarteriole is a type of vessel that has structural characteristics of both an arteriole and a capillary. Slightly larger than the typical capillary, the smooth muscle of the tunica media of the metarteriole is non continuous but forms rings of smooth muscle (sphincters) prior to the archway to the capillaries. Each metarteriole arises from a concluding arteriole and branches to supply blood to a capillary bed that may consist of ten–100 capillaries.
The precapillary sphincters, round smooth muscle cells that surround the capillary at its origin with the metarteriole, tightly regulate the flow of blood from a metarteriole to the capillaries it supplies. Their function is critical: If all of the capillary beds in the body were to open up simultaneously, they would collectively hold every drop of blood in the trunk and at that place would be none in the arteries, arterioles, venules, veins, or the eye itself. Unremarkably, the precapillary sphincters are closed. When the surrounding tissues need oxygen and take excess waste products, the precapillary sphincters open up, allowing blood to flow through and exchange to occur before closing once more (see Figure 5). If all of the precapillary sphincters in a capillary bed are airtight, blood will flow from the metarteriole directly into a thoroughfare aqueduct and and then into the venous apportionment, bypassing the capillary bed entirely. This creates what is known equally a vascular shunt. In addition, an arteriovenous anastomosis may bypass the capillary bed and lead straight to the venous organization.
Although you lot might await claret flow through a capillary bed to be polish, in reality, it moves with an irregular, pulsating menstruum. This pattern is called vasomotion and is regulated by chemic signals that are triggered in response to changes in internal conditions, such as oxygen, carbon dioxide, hydrogen ion, and lactic acid levels. For example, during strenuous practice when oxygen levels decrease and carbon dioxide, hydrogen ion, and lactic acid levels all increase, the capillary beds in skeletal musculus are open, equally they would be in the digestive system when nutrients are present in the digestive tract. During slumber or balance periods, vessels in both areas are largely airtight; they open only occasionally to let oxygen and nutrient supplies to travel to the tissues to maintain basic life processes.

Effigy 5. In a capillary bed, arterioles requite rise to metarterioles. Precapillary sphincters located at the junction of a metarteriole with a capillary regulate blood menstruation. A thoroughfare channel connects the metarteriole to a venule. An arteriovenous anastomosis, which direct connects the arteriole with the venule, is shown at the bottom.
Venules
A venule is an extremely small vein, by and large eight–100 micrometers in diameter. Postcapillary venules join multiple capillaries exiting from a capillary bed. Multiple venules join to form veins. The walls of venules consist of endothelium, a sparse center layer with a few muscle cells and elastic fibers, plus an outer layer of connective tissue fibers that constitute a very thin tunica externa. Venules equally well as capillaries are the primary sites of emigration or diapedesis, in which the white blood cells attach to the endothelial lining of the vessels and and so squeeze through adjacent cells to enter the tissue fluid.
Veins
A vein is a blood vessel that conducts claret toward the heart. Compared to arteries, veins are thin-walled vessels with big and irregular lumens (see Figure 6).

Figure 6. Many veins take valves to prevent dorsum menses of blood, whereas venules do not. In terms of scale, the diameter of a venule is measured in micrometers compared to millimeters for veins.
Considering they are low-pressure vessels, larger veins are commonly equipped with valves that promote the unidirectional menses of blood toward the middle and preclude backflow toward the capillaries caused by the inherent depression blood pressure in veins too as the pull of gravity. Table ii compares the features of arteries and veins.
| Table 2. Comparison of Arteries and Veins | ||
|---|---|---|
| Arteries | Veins | |
| Management of blood catamenia | Conducts blood abroad from the middle | Conducts blood toward the heart |
| General advent | Rounded | Irregular, often complanate |
| Pressure level | High | Low |
| Wall thickness | Thick | Thin |
| Relative oxygen concentration | Higher in systemic arteries Lower in pulmonary arteries | Lower in systemic veins Higher in pulmonary veins |
| Valves | Not nowadays | Nowadays most normally in limbs and in veins inferior to the heart |
Disorders of the Cardiovascular Arrangement: Edema and Varicose Veins
Despite the presence of valves and the contributions of other anatomical and physiological adaptations we will cover shortly, over the course of a 24-hour interval, some blood will inevitably pool, peculiarly in the lower limbs, due to the pull of gravity. Whatsoever blood that accumulates in a vein will increase the pressure within it, which can then be reflected back into the smaller veins, venules, and somewhen even the capillaries. Increased force per unit area will promote the flow of fluids out of the capillaries and into the interstitial fluid. The presence of excess tissue fluid around the cells leads to a condition chosen edema.
Near people experience a daily accumulation of tissue fluid, especially if they spend much of their work life on their feet (like most health professionals). However, clinical edema goes beyond normal swelling and requires medical treatment. Edema has many potential causes, including hypertension and center failure, astringent protein deficiency, renal failure, and many others. In order to treat edema, which is a sign rather than a discrete disorder, the underlying crusade must be diagnosed and alleviated.

Figure 7. Varicose veins are commonly found in the lower limbs. (credit: Thomas Kriese)
Edema may be accompanied by varicose veins, peculiarly in the superficial veins of the legs. This disorder arises when lacking valves allow blood to accumulate within the veins, causing them to distend, twist, and become visible on the surface of the integument. Varicose veins may occur in both sexes, merely are more common in women and are often related to pregnancy. More than than simple cosmetic blemishes, varicose veins are often painful and sometimes itchy or throbbing. Without handling, they tend to grow worse over time. The utilize of support hose, likewise as elevating the anxiety and legs whenever possible, may be helpful in alleviating this condition. Laser surgery and interventional radiologic procedures tin reduce the size and severity of varicose veins. Severe cases may require conventional surgery to remove the damaged vessels. As there are typically redundant apportionment patterns, that is, anastomoses, for the smaller and more superficial veins, removal does non typically impair the circulation. There is prove that patients with varicose veins suffer a greater hazard of developing a thrombus or clot.
Veins as Blood Reservoirs
In addition to their primary part of returning blood to the eye, veins may be considered claret reservoirs, since systemic veins contain approximately 64 percent of the blood volume at any given time. Their ability to concur this much claret is due to their high capacitance, that is, their chapters to distend (expand) readily to shop a high volume of blood, fifty-fifty at a low pressure. The large lumens and relatively sparse walls of veins make them far more distensible than arteries; thus, they are said to be capacitance vessels.
Summary: Distribution of Blood Flow
The following list breaks downwards the blood flow throughout the body:
- Systemic circulation 84%
- Systemic veins 64%
- Large veins 18%
- Large venous networks (liver, bone marrow, and integument) 21%
- Venules and medium sized veins 25%
- Systemic arteries 13%
- Arterioles ii%
- Muscular arteries 5%
- Elastic arteries 4%
- Aorta 2%
- Systemic capillaries seven%
- Systemic veins 64%
- Pulmonary apportionment 9%
- Pulmonary veins 4%
- Pulmonary arteries 3%
- Pulmonary capillaries two%
- Middle seven%
When blood flow needs to be redistributed to other portions of the body, the vasomotor centre located in the medulla oblongata sends sympathetic stimulation to the polish muscles in the walls of the veins, causing constriction—or in this case, venoconstriction. Less dramatic than the vasoconstriction seen in smaller arteries and arterioles, venoconstriction may be likened to a "stiffening" of the vessel wall. This increases pressure on the blood within the veins, speeding its return to the heart. As you will note in the image above, approximately 21 percent of the venous claret is located in venous networks inside the liver, os marrow, and integument. This volume of blood is referred to as venous reserve. Through venoconstriction, this "reserve" book of claret can get back to the heart more than chop-chop for redistribution to other parts of the apportionment.
Careers in Action: Vascular Surgeons and Technicians
Vascular surgery is a specialty in which the physician deals primarily with diseases of the vascular portion of the cardiovascular system. This includes repair and replacement of diseased or damaged vessels, removal of plaque from vessels, minimally invasive procedures including the insertion of venous catheters, and traditional surgery. Post-obit completion of medical school, the physician generally completes a v-twelvemonth surgical residency followed past an boosted 1 to 2 years of vascular specialty preparation. In the United States, nigh vascular surgeons are members of the Society of Vascular Surgery.
Vascular technicians are specialists in imaging technologies that provide information on the health of the vascular system. They may likewise assist physicians in treating disorders involving the arteries and veins. This profession ofttimes overlaps with cardiovascular technology, which would as well include treatments involving the middle. Although recognized by the American Medical Association, in that location are currently no licensing requirements for vascular technicians, and licensing is voluntary. Vascular technicians typically have an Acquaintance's degree or certificate, involving 18 months to 2 years of training. The Us Bureau of Labor projects this profession to grow by 29 percent from 2010 to 2020.
- Visit this site to learn more virtually vascular surgery.
- Visit this site to acquire more near vascular technicians.
Chapter Review
Claret pumped by the heart flows through a serial of vessels known equally arteries, arterioles, capillaries, venules, and veins earlier returning to the heart. Arteries transport blood away from the centre and branch into smaller vessels, forming arterioles. Arterioles distribute blood to capillary beds, the sites of exchange with the body tissues. Capillaries lead dorsum to modest vessels known equally venules that flow into the larger veins and eventually back to the centre.
The arterial system is a relatively high-pressure system, so arteries take thick walls that announced circular in cantankerous section. The venous organisation is a lower-pressure organization, containing veins that accept larger lumens and thinner walls. They oft appear flattened. Arteries, arterioles, venules, and veins are equanimous of three tunics known as the tunica intima, tunica media, and tunica externa. Capillaries accept only a tunica intima layer. The tunica intima is a thin layer composed of a elementary squamous epithelium known as endothelium and a pocket-size amount of connective tissue. The tunica media is a thicker area composed of variable amounts of smoothen muscle and connective tissue. It is the thickest layer in all only the largest arteries. The tunica externa is primarily a layer of connective tissue, although in veins, it too contains some shine muscle. Claret menstruation through vessels can be dramatically influenced by vasoconstriction and vasodilation in their walls.
Self Cheque
Answer the question(due south) below to come across how well you understand the topics covered in the previous section.
Critical Thinking Questions
- Arterioles are often referred to as resistance vessels. Why?
- Cocaine use causes vasoconstriction. Is this likely to increase or subtract blood force per unit area, and why?
- A blood vessel with a few smooth muscle fibers and connective tissue, and only a very thin tunica externa conducts blood toward the middle. What type of vessel is this?
Glossary
arteriole:(besides, resistance vessel) very small artery that leads to a capillary
arteriovenous anastomosis:short vessel connecting an arteriole directly to a venule and bypassing the capillary beds
avenue:blood vessel that conducts blood away from the heart; may be a conducting or distributing vessel
capacitance:power of a vein to distend and store blood
capacitance vessels:veins
capillary:smallest of blood vessels where physical substitution occurs between the blood and tissue cells surrounded by interstitial fluid
capillary bed:network of 10–100 capillaries connecting arterioles to venules
continuous capillary:nearly common blazon of capillary, found in nigh all tissues except epithelia and cartilage; contains very small gaps in the endothelial lining that allow commutation
rubberband artery:(likewise, conducting artery) avenue with abundant rubberband fibers located closer to the centre, which maintains the pressure gradient and conducts claret to smaller branches
external elastic membrane:membrane composed of elastic fibers that separates the tunica media from the tunica externa; seen in larger arteries
fenestrated capillary:type of capillary with pores or fenestrations in the endothelium that permit for rapid passage of certain small materials
internal elastic membrane:membrane composed of elastic fibers that separates the tunica intima from the tunica media; seen in larger arteries
lumen: interior of a tubular structure such every bit a blood vessel or a portion of the alimentary culvert through which blood, chyme, or other substances travel
metarteriole:curt vessel arising from a terminal arteriole that branches to supply a capillary bed
microcirculation:blood flow through the capillaries
muscular artery:(besides, distributing artery) artery with arable smooth muscle in the tunica media that branches to distribute blood to the arteriole network
nervi vasorum:small nervus fibers plant in arteries and veins that trigger contraction of the smoothen muscle in their walls
perfusion:distribution of blood into the capillaries and so the tissues can be supplied
precapillary sphincters:round rings of smooth muscle that surround the entrance to a capillary and regulate blood flow into that capillary
sinusoid capillary:rarest type of capillary, which has extremely large intercellular gaps in the basement membrane in addition to clefts and fenestrations; found in areas such as the bone marrow and liver where passage of large molecules occurs
thoroughfare channel:continuation of the metarteriole that enables claret to bypass a capillary bed and flow straight into a venule, creating a vascular shunt
tunica externa:(besides, tunica adventitia) outermost layer or tunic of a vessel (except capillaries)
tunica intima:(also, tunica interna) innermost lining or tunic of a vessel
tunica media:centre layer or tunic of a vessel (except capillaries)
vasa vasorum:small blood vessels located within the walls or tunics of larger vessels that supply nourishment to and remove wastes from the cells of the vessels
vascular shunt:continuation of the metarteriole and thoroughfare aqueduct that allows blood to bypass the capillary beds to flow directly from the arterial to the venous circulation
vasoconstriction:constriction of the smooth muscle of a blood vessel, resulting in a decreased vascular bore
vasodilation:relaxation of the smoothen muscle in the wall of a blood vessel, resulting in an increased vascular diameter
vasomotion:irregular, pulsating period of blood through capillaries and related structures
vein:blood vessel that conducts blood toward the middle
venous reserve:volume of blood contained inside systemic veins in the integument, bone marrow, and liver that tin be returned to the heart for apportionment, if needed
venule:small vessel leading from the capillaries to veins
Source: https://courses.lumenlearning.com/suny-ap2/chapter/structure-and-function-of-blood-vessels/
0 Response to "What Layer Can Change Blood Vessel Diameter by Vasodilation and Vasoconstriction?"
Post a Comment